Where Is the Evidence?
Recent risk communications from CDC , FDA, and USDA regarding transmission of highly pathogenic avian influenza virus or HPAI (subtype H5N1) to humans via raw milk include no supporting evidence of viral transmission from raw milk to humans in the peer-reviewed literature. CDC and USDA reported that the HPAI strains recently isolated in the US lack the genetic markers for viruses adapted to infect humans. An extensive body of scientific evidence from the peer-reviewed literature introduced herein does not support the assumption by these US government agencies that HPAI transmits to humans via milkborne or foodborne routes and causes disease. Nor does the scientific evidence support the recommendation that consumers should avoid raw milk and raw milk products.
In March of 2024, dead wild birds on a TX dairy farm and unusual symptoms in older dairy cows (decreased lactation, low appetite, other clinical signs) triggered sampling of affected cows (oropharyngaeal swabs) and their milk. On March 25th, Texas Animal Health Commission confirmed samples were positive for HPAI. A dairy worker on this farm with eye inflammation was also confirmed positive for HPAI, though it is unclear if the worker had contact with both the dead birds and the affected cows.
On April 9th, the World Health Organization (WHO) stated the following about the TX case. “This is the first human infection with [HPAI (H5N1)] acquired from contact with infected cattle and the second confirmed human case of influenza A(H5N1) detected in the country. No additional associated cases of human infection with influenza A(H5N1) have been identified. Since the virus has not acquired mutations that facilitate transmission among humans and based on available information, WHO assesses the public health risk to the general population posed by this virus to be low and for occupationally exposed persons, the risk of infection is considered low-to-moderate.“ In addition, the American Association of Bovine Practitioners (AABP) now recommends a new name, Bovine Influenza A Virus (BIAV) because the virus is not highly pathogenic in dairy cows.
The WHO lists the following factual information about avian influenza: i) “Direct contact with infected animals (through handling, culling, slaughtering or processing) or indirect contact (through environments contaminated with bodily fluids from infected animals) represent a risk for human infection.“; ii) “animal influenza viruses are distinct from human influenza viruses and do not easily transmit to and among humans;” and iii) sustained person-to-person transmission is not demonstrated.
Of all the transmission sources reported in surveillance systems by CDC and other government agencies (animal contact, environmental, foodborne, person-to-person, and waterborne), the only demonstrated transmission source for HPAI transmission to humans is animal contact. In light of the body of evidence on HPAI transmission to humans by direct animal contact, not by foodborne transmission, risk communications to avoid consumption of raw milk and raw milk products do not appear to be based on scientific evidence, but on other factors.
An earlier risk assessment conducted by FDA and USDA (2010) determined that HPAI “is not considered to be a foodborne pathogen although virus had been isolated from poultry muscle and the interior of eggs”. This is consistent with current facts compiled by the WHO about avian influenza transmission to date: i) “Direct contact with infected animals (through handling, culling, slaughtering or processing) or indirect contact (through environments contaminated with bodily fluids from infected animals) represent a risk for human infection.“; ii) “animal influenza viruses are distinct from human influenza viruses and do not easily transmit to and among humans;” and iii) “sustained person-to-person transmission is not demonstrated”. Although HPAI was detected in milk from ill cows in TX, as in poultry muscle and eggs, no evidence supports foodborne transmission of HPAI to humans.
While no evidence supports milkborne or foodborne transmission of HPAI to humans, evidence does exist that demonstrates a multitude of well-characterized mechanistic factors that inactivate viruses and prevent foodborne illness. Key studies in the peer-reviewed literature are cited in brackets, with full references appended.
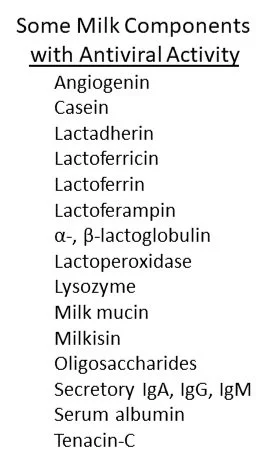
First, consider peer-reviewed studies demonstrating antiviral properties of a suite of bioactive components of raw mammalian milks, including bovine milk [4,5,7-9,12-14,16,17,19]. Multiple researchers note that some of the antiviral components of milk listed in the text box below are likely function synergistically, meaning effects are greater in combination than independently, an observation particularly relevant in complex gut ecosystems of humans that include innate and adaptive immune systems. Many of these bioactive components of raw milk are also sensitive to heat and may be absent, inactive, or present in lower concentrations in pasteurized milks. Considering the extensive literature on antiviral activity in milk, clinical researchers [3] applied deep scientific knowledge to recommend that infants not be deprived of raw breastmilk due to the presence of viruses. The benefits of feeding raw breastmilk including its antiviral components to infants outweighs the very small risk of infection, from their perspective as clinical researchers, one associated with the Italian Association of Human Milk Banks.
Next, consider the gauntlet of defenses against foodborne pathogens in the human digestive tract [1,6,18]. These defenses include physical (stomach acidity, peristalsis), chemical (digestive enzymes), and cellular (innate and adaptive immune system, microbiota) factors that, acting simultaneously or sequentially, inactivate pathogens, including viruses, and/or suppress infectivity and virulence of ingested pathogens. Researchers [11] note that HPAI is an enveloped virus, susceptible to disruption and degradation in stomach acids, unlike the 16 viruses known to be transmitted to human by the oral route [6]. Further, FDA and USDA determined in 2010 that HPAI “is not considered to be a foodborne pathogen” even though virus was isolated from poultry muscle and the interior of eggs.
Host chemical and cellular defenses include: complement; defensins; enzymes; interferons; interleukins; pattern recognition receptors (Toll-like receptors 3, 4, and 7; NOD-like receptors; RIG-1 receptors); and an array of host cells (dendritic cells, B cells, intestinal epithelial cells, macrophages, monocytes, natural killer cells, T cells) and cells of the gut-associated microbes or microbiota. Also, the gut microbiota include not only commensal (non-pathogenic) bacteria, but also commensal viruses that can modulate infectivity and virulence of pathogens [10].
Now, consider that the microbial ecology of raw milks including antiviral activity as described briefly above aligns with recent CDC data for all transmission sources from 2005 to 2020 [15]. This CDC dataset included 3,807 milkborne illnesses (2,111 associated with pasteurized milk) linked to bacterial pathogens, but lacks any viral illness associated with milk, raw or pasteurized. The predominant virus in this CDC dataset was norovirus, associated with 8,199 illnesses from leafy greens reported over this 16-year period. No norovirus illnesses or any other viral illnesses were reported in milk.
What is known about HPAI transmission to humans is that it is rare, requiring prolonged direct contact with infected, sick, and dead animals, generally birds, now dairy cows, that can lead to mild flu-like symptoms or eye inflammation, some progressing to fatal infections, according to WHO. Again, HPAI in humans is linked to transmission via animal contact, not by foods.
It seems that occupational exposure resulted in infection of a farm worker handling ill cows, with developed of one symptom in the worker, eye redness (conjunctivitis), consistent with transmission by animal contact. HPAI has been detected in dairy cows in Texas, Kansas, New Mexico and Michigan as of April 2. The dairy animals and rare humans affected have recovered.
Cross-disciplinary evidence demonstrates that raw milk from healthy cows is not inherently dangerous, consistent with the CDC evidence of trends for 2005-2020 [15] and evidence of benefits and risks [2]. There is no scientific evidence that HPAI in raw milk causes human disease.
Please consider the references below and pose questions in the comments. Also stay tuned for my next blogs on our recent peer-reviewed publications.
Trends in burdens of disease by transmission source (usa, 2005–2020) and hazard identification for foods: focus on milkborne disease.
Journal of Epidemiology and Global Health.Suppression of pathogens in properly refrigerated raw milk.
PLOS ONELessons identified from applications of the Risk Analysis Quality Test Release 1.0.
Risk Analysis
References
1. Buchanan RL, Havelaar AH, Smith MA, Whiting RC, Julien E. The key events dose-response framework: its potential for application to foodborne pathogenic microorganisms. Critical Reviews in Food Science and Nutrition. 2009 Sep 22;49(8):718-28.
2. Dietert RR, Coleman ME, North DW, Stephenson MM. Nourishing the human holobiont to reduce the risk of non-communicable diseases: a cow’s milk evidence map example. Applied Microbiology. 2021 Dec 30;2(1):25-52.
3. Francese R, Peila C, Donalisio M, Lamberti C, Cirrincione S, Colombi N, Tonetto P, Cavallarin L, Bertino E, Moro GE, Coscia A. Viruses and human milk: transmission or protection?. Advances in Nutrition. 2023 Aug 20.
4. Gallo V, Giansanti F, Arienzo A, Antonini G. Antiviral properties of whey proteins and their activity against SARS-CoV-2 infection. Journal of Functional Foods. 2022 Feb 1;89:104932.
5. Gallo V, Arienzo A, Tomassetti F, Antonini G. Milk bioactive compounds and gut microbiota modulation: the role of whey proteins and milk oligosaccharides. Foods. 2024 Mar 16;13(6):907.
6. Lockhart A, Mucida D, Parsa R. Immunity to enteric viruses. Immunity. 2022 May 10;55(5):800-18.
7. Kaplan M, Şahutoğlu AS, Sarıtaş S, Duman H, Arslan A, Pekdemir B, Karav S. Role of milk glycome in prevention, treatment, and recovery of COVID-19. Frontiers in Nutrition. 2022 Nov 8;9:1033779.
8. Oda H, Kolawole AO, Mirabelli C, Wakabayashi H, Tanaka M, Yamauchi K, Abe F, Wobus CE. Antiviral effects of bovine lactoferrin on human norovirus. Biochemistry and Cell Biology. 2021;99(1):166-72.
9. Panon G, Tache S, Labie C. Antiviral substances in raw bovine milk active against bovine rotavirus and coronavirus. Journal of Food Protection. 1987 Oct 1;50(10):862-7.
10. Pavia G, Marascio N, Matera G, Quirino A. Does the human gut virome contribute to host health or disease?. Viruses. 2023 Nov 17;15(11):2271.
11. Sangsiriwut K, Uiprasertkul M, Payungporn S, Auewarakul P, Ungchusak K, Chantratita W, Puthavathana P. Complete Genomic Sequences of Highly Pathogenic H5N1 Avian Influenza Viruses Obtained Directly from Human Autopsy Specimens. Microbiol Resour Announc. 2018. 7(22):e01498-18. doi: 10.1128/MRA.01498-18. PMID: 30533850; PMCID: PMC6284082.
12. Santos I, Silva M, Grácio M, Pedroso L, Lima A. Milk antiviral proteins and derived peptides against zoonoses. International Journal of Molecular Sciences. 2024. 25(3):1842.
13. Schlusselhuber M, Godard J, Sebban M, Bernay B, Garon D, Seguin V, Oulyadi H, Desmasures N. Characterization of milkisin, a novel lipopeptide with antimicrobial properties produced by Pseudomonas sp. UCMA 17988 isolated from bovine raw milk. Frontiers in Microbiology. 2018. 9:355822.
14. Singh P, Hernandez‐Rauda R, Peña‐Rodas O. Preventative and therapeutic potential of animal milk components against COVID‐19: A comprehensive review. Food Science & Nutrition. 2023. 11(6):2547-79.
15. Stephenson MM, Coleman ME, Azzolina NA. Trends in burdens of disease by transmission source (USA, 2005–2020) and hazard identification for foods: focus on milkborne disease. Journal of Epidemiology and Global Health. 2024 Mar 28:1-30.
16. Tache S, Benkaddour M, Corpet DE. Rotavirus inhibitor and recovery in raw bovine milk. Journal of Food Protection. 1995 Apr 1;58(4):434-8.
17. Taha SH, Mehrez MA, Sitohy MZ, Abou Dawood AG, Abd-El Hamid MM, Kilany WH. Effectiveness of esterified whey proteins fractions against Egyptian Lethal Avian Influenza A (H5N1). Virology Journal. 2010 Dec;7:1-4.
18. Wan T, Wang Y, He K, Zhu S. Microbial sensing in the intestine. Protein & Cell. 2023 Nov 1;14(11):824-60.
19. Wang X, Yue L, Dang L, Yang J, Chen Z, Wang X, Shu J, Li Z. Role of sialylated glycans on bovine lactoferrin against influenza virus. Glycoconjugate Journal. 2021 Dec 1:1-8.