REOPENING NY SPORTS/ RECREATION GUIDELINES TO MINIMIZE COVID-19 RISKS
AEROSOL TRANSMISSION, QMRA, COMPOUND HAZARDS: WEAR YOUR MASK!
I never imagined that I would be preparing a 5th blog on a viral pandemic this year, but I believe that risk practitioners have great value to contribute to deliberations of how to assess and communicate risks and benefits, and manage risk tradeoffs, in these difficult, uncertain times. Kudos to those experts from the Society for Risk Analysis (SRA) who are contributing critical interdisciplinary perspectives that are sorely needed to develop appropriate tradeoffs for health and economic and social risks that communities, nations, and the world are suffering as the COVID-19 pandemic caused by the novel corona virus SARS-CoV-2 illustrated below continues to spread around the world.
https://en.wikipedia.org/wiki/Coronavirus_disease
This blog covers experiences applying the Reopening NY Sports and Recreation Guidelines to minimize risks, new studies on inactivation of the novel corona virus (SARS-CoV-2) by simulated sunlight and a comprehensive Quantitative Microbial Risk Assessment (QMRA) for indoor and outdoor exposures to viral aerosols, and podcasts from more episodes of the SRA COVID Conversations on Risk series.
Some Issues on Reopening Outdoor Sports
Even people who know me may not know that I work out with the Ithaca Dragon Boat Club (IDBC) here in beautiful upstate NY. IDBC members practice Monday, Wednesday, and Saturday on the longest and second deepest of NY’s Finger Lakes (Cayuga Lake, ~40 miles long).
For the first two months this year, members paddled kayaks and canoes, not our dragon boats. If you have not seen a dragon boat or a race, the risks may not be obvious. Here is a photo of the IDBC competing in a boat at last year’s Chatauqua Lake Dragon Boat Race, and another of the medal brought home by each of the 22 team members.
After you view the photo below, the risks are obvious. A full dragon boat has 20 paddlers in 10 pairs, cheek to cheek, plus a drummer and a person to steer. So, a team of 22 people in close contact, breathing hard, some mouth breathing, would assume some risks without making adjustments for COVID-19.
Our boats are docked outdoors in an Ithaca City Park, and all users of Ithaca City and NY State Parks, including IDBC members, wear masks or face shields to protect themselves and others when the six-foot social distancing limit cannot be maintained. So, no races and no medals like this one from the Chatauqua Lake race are likely for the 2020 season.
IDBC now has procedures specifying the adjustments we are making for COVID-19 this season, as well as a NY Forward Safety Plan. Any member who has symptoms or traveled within 14 days prior does not practice. Travelers outside of largely rural Tompkins County in upstate NY (where <200 residents tested positive and none have died during the pandemic so far) can return to practice after 14 days of symptom-free quarantine.
The IDBC’s two new boats, the Osprey and the Taughannock, left the dock for the first time this weekend with masked paddlers. Members signed up in advance on the Team App for an assigned seat on a dragon boat, with one member steering. Other members continued to paddle individually, in kayaks, canoes, outrigger canoes, and stand up paddleboards (SUPs). IDBC is committed to following these guidelines and procedures to protect our health and the health of our community.
Where’s the Science? The Risk Analysis?
This week, I shared two newly published studies with IDBC members that are relevant to our practices.
Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces (Ratnesar-Shumate et al., 2020)
Infection Risk Assessment of COVID-19 through Aerosol Transmission: a Case Study of South China Seafood Market (Zhang et al., 2020)
The first study, conducted by researchers at the National Biodefense Analysis and Countermeasures Center (NBACC) in MD, found that 90% of the novel corona virus in simulated saliva (mimicking respiratory droplets) was inactivated within 7 minutes in simulated sunlight. Thus, IDBC leaders consider that disinfection of the boats between practices is not warranted at present. However, disinfectant is provided if paddlers prefer extra protection. Paddlers will not share water bottles, paddles, or life preservers, and will be assigned, one per seat, on alternate sides of the boat for proper balance while minimizing potential exposures via physical contact and exhaled air.
The second study was shared with me by SRA Fellow and Drexel University Professor Charles Haas. Zhang and colleagues integrated available data on SARS-CoV-2 (or data on related corona viruses as potential surrogates) and made assumptions to model hypothetical risk scenarios for potential transmissions at the Wuhan South China Seafood Market.
For example, although data on viral shedding from infected persons and aerosol transmission are not available from the market early in the pandemic, laboratory data on viral replication in tissue culture cells was used to estimate the potential load of viral shedding from an infected worker. Detailed models were developed to simulate potential dispersion of virus from one infected worker through indoor air with models for biologic decay, lung deposition for those inhaling contaminated air, and infection of others working or shopping in this specific indoor environment with minimal ventilation. Further, potential dispersion of contaminated air exiting the building into outdoor air was modeled for various distances outside the exits of the building. The simulation approach and results are illustrated below.
The dispersion model predicted that contaminated air exiting the building by natural ventilation is rapidly diluted, with dispersion into high altitudes well outside the breathing zone of simulated pedestrians as distance increased from the exits of the market. Risk estimates decreased by 100-fold for pedestrians 600 meters away from the market, relative to someone at the exit before dispersion of contaminated air. The predominant uncertainties noted by the researchers were the models for estimating likelihood of illness at inhaled viral doses or viral loads (dose-response modeling), viral shedding from infected persons, and biological decay (e.g., desiccation and inactivation via multiple factors).
What We Don’t Know
From these studies and other evidence discussed by SRA experts in the COVID Conversations on Risk series, we do not know:
what viral doses (viral loads) in the exhaled breath, sneezes or coughs of an infected person are necessary before that person sheds virus and becomes infectious to others;
what viral doses (viral loads) are necessary for inhalation, infection, and progression to illness in persons with variable susceptibility factors; and
how likely such viral doses are within the breathing zone of dragon boat paddlers sitting on average 4.5 feet apart (or even 6 feet apart) under variable outdoor conditions of sun, wind, rain, and spray.
What Do SRA Experts Have to Say?
Click on the link below to view the 1-hour podcast of Episode 9 of the SRA COVID Conversations on Risk series, considering aerosol transmission and implications for public health. The speakers are two esteemed SRA Fellows, both recipients of the SRA Presidential Recognition Award: Drs. Elizabeth Anderson of Exponent and Charles Haas of Drexel University. Dr. Anderson is a Past President of SRA and RJ Burk Outstanding Service Award recipient. Dr. Haas serves as area editor for Microbial Risk Assessment for the SRA journal Risk Analysis.
Dr. Anderson shared this review published in Annals of Internal Medicine that includes summaries of the available evidence on asymptomatic transmission.
Prevalence of Asymptomatic SARS-CoV-2 Infection : A Narrative Review (Oran and Topol, 2020)
Click on the link below to listen to the 30-minute podcast of Episode 10 of the SRA COVID Conversations on Risk series, on compound hazards (pandemic and floods, fires, hurricanes) by Drs. Robyn Wilson of The Ohio State University and Gina Eosco of the National Oceanic and Atmospheric Administration. Dr. Wilson is a recipient of the Chauncey Starr Distinguished Young Analyst Award. Dr. Eosco is another distinguished young analyst who spoke at an Upstate NY SRA event while she was a student at nearby Cornell University, studying with former SRA President Katherine McComas.
Thank you to these SRA experts and all those who contribute to COVID Conversations on Risk.
Bottom Line: WEAR YOUR MASK!
Uncertainties still exist, even in areas where the rates of new cases seem to be declining. Since we cannot predict who may be infectious in a crowd, whether or not they tested positive or have symptoms, protect yourself and others by masking and complying with guidance as our communities work their way back to full recovery.
NOT SURE YOU BELIEVE CLOTH MASKS ARE EFFECTIVE?
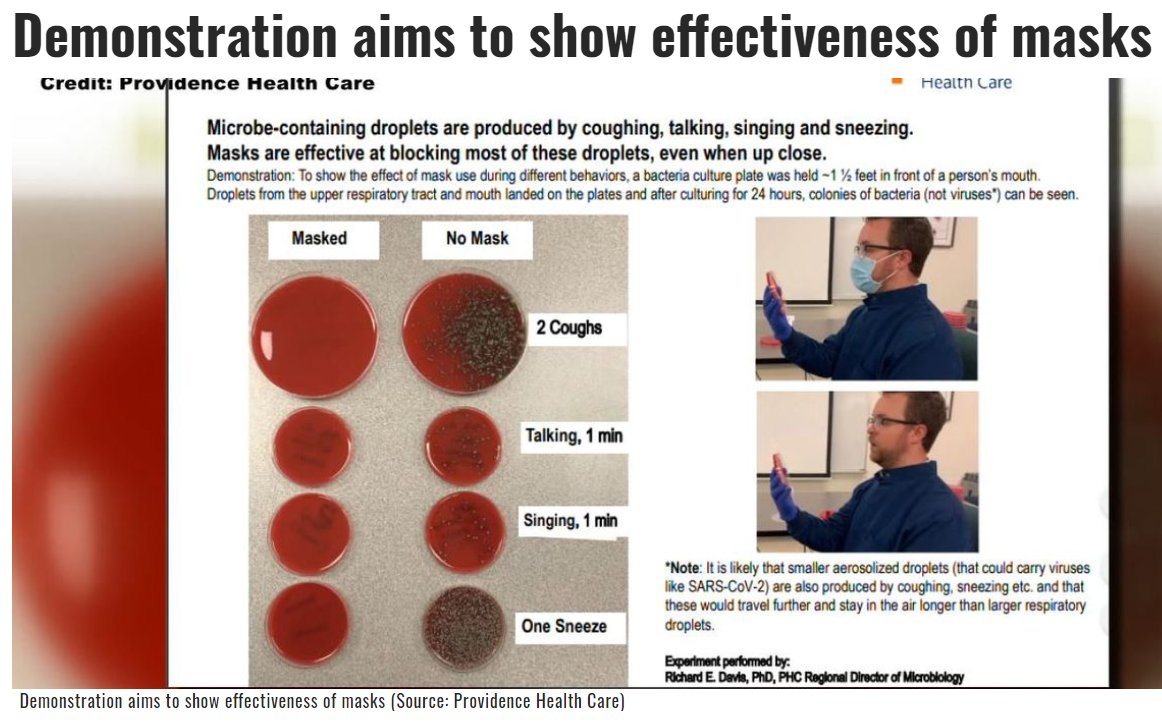
Dr. Rich Davis, Director of the Microbiology Lab at Providence Health Care, demonstrated that a simple cloth surgical style mask is effective at blocking most respiratory droplets relevant to spread of COVID-19. Although viral particles may be dispersed farther than the bacteria cultured on the plates in Dr. Davis’s experiment, his results demonstrate a point made during the COVID Conversations on Risk webinar above by Dr. Haas: masks do not need to be perfect (e.g., N95 respirator with very close facial fit and very efficient filtration of airborne particles) to physically trap microbes in exhaled air from talking, singing, coughing, and sneezing. Growth is obviously higher after coughing and sneezing than talking or singing, consistent with higher risk of COVID transmission for those exposed to coughing and sneezing of symptomatic cases.
WEAR A MASK to reduce risks to yourself and others around you.
https://www.wbtv.com/2020/06/29/demonstration-aims-show-effectiveness-masks/